The PCR test, formally known as the Polymerase Chain Reaction, is the technology used around the world to detect SARS-CoV-2, the virus that causes COVID-19. The PCR test is defined as a test to detect genetic material from a specific organism, such as a virus. The test detects the presence of a virus if you have the virus at the time of the test. The test could also detect fragments of the virus even after you are no longer infected. In the context of COVID-19, labs use the PCR technology to amplify small amounts of RNA from specimens into DNA, which is replicated until SARS-CoV-2 is detectable, if present. Each replication of the sample is also called a cycle. The number of cycles required before the virus is detectable from the sample is called the cycle threshold. The higher the number of cycles required to detect the virus, the less virus there is in the sample. It's important to note the distinction between a positive PCR result, and an infectious case of COVID-19. A PCR test is not a diagnostic tool and cannot tell anything about the person who the sample came from, other than some amount of genetic material unique to SARS-CoV-2 was present.
It's the position of the NSCLA that, while the PCR test is incredibly accurate at detecting whatever genetic material is being tested for, the way it is being used to drive public policy around COVID-19 is an overly simplified, one size fits all solution that simply doesn't work in its current form. This is because a significant portion of positive PCR tests do not relate to a person who is sick or infectious. Yet cycle threshold does not currently play any role in COVID-19 policy, meaning the requirement to isolate, stay home from work etc... is not tailored in any way to the information available from a PCR test, even though there is robust information that could guide policy in the real world. Why? Let's look at the science.

PCR Cycle Threshold Value is Proportional to Viral Load (Infectiousness)
This study in the Clinical Infectious Diseases journal from September 2020 did the necessary analysis on thousands of positive PCR test results. They attempted to culture live virus from each sample in the study. The ability to culture live virus from a sample indicates whether there is in fact live virus capable of being infectious, vs dead or inactive genetic material that is of no harm to anyone. The results were clear, at 25 PCR cycles, about 70% of samples had live virus. However, at 30 cycles, that drops to just 20%, meaning 80% of all samples had no live virus. At 35 cycles, less than 3% of samples had live virus, meaning over 97% did not. The study also concludes that even where there is live virus, the viral load (the amount of live virus) goes down the higher the cycle threshold required to detect it.
These results have massive implications, because currently, regardless of whether you test positive at 10 or 40 cycles, you are treated exactly the same, even though the risk you pose to yourself and the public is wildly different. At this stage in the pandemic, we need to be using this readily available data to inform a more nuanced approach to public policy that allows us to safely live with COVID-19 and understand that every positive PCR result is not equal.
56% of Positive “Cases” are Not Infectious
Manitoba Chief Microbiologist and Laboratory Specialist Dr. Jared Bullard confirms while testifying under oath in a case brought by the Justice Centre for Constitutional Freedoms, that PCR test results do not verify infectiousness, and were never intended to be used to diagnose respiratory illnesses. He goes on to testify that while a person with Covid-19 is infectious for a one-to-two week period, non-viable (harmless) viral SARS-CoV-2 fragments remain in the nose, and can be detected by a PCR test for up to 100 days after exposure. A study from Dr. Bullard and his colleagues found that only 44% of positive PCR test results would actually grow in the lab, meaning 56% of positive results are unlikely to be infectious, and these were samples using a cycle threshold of just 18. Dr. Bullard confirmed that he has never been able to culture live virus from any sample where the cycle threshold was 25 or higher. In Canada, PCR tests will run until as many as 45 cycles have been reached before a negative result is confirmed.
Up to 90% of Positive “Cases” are Not Infectious
The NY Times released an article back in August of 2020 reporting on data that was released by officials in Massachusetts, New York and Nevada. They found that around 90% of all samples that had a positive PCR test result carried so little virus, those people should not be required to submit to contact tracing or self isolation as they would not be contagious. "Tests with thresholds so high may detect not just live virus but also genetic fragments, leftovers from infection that pose no particular risk — akin to finding a hair in a room long after a person has left," Dr. Mina said. "Any test with a cycle threshold above 35 is too sensitive," agreed Juliet Morrison, a virologist at the University of California, Riverside. “I’m shocked that people would think that 40 (cycle threshold) could represent a positive,” she said. Dr. Mina also said that she would set the cycle threshold at 30, or even less. Reducing the threshold from 40 to 30 would mean the amount of genetic material in a patient’s sample would have to be 100-fold to 1,000-fold lower than that of the current standard for the test to return a positive result. The CDC themselves suggested that is it extremely difficult to detect any live virus in a sample above a threshold of 33 cycles
Officials at the Wadsworth Center, New York’s state lab, have access to cycle threshold values from tests they have processed, and analyzed them at The Times’s request. In July, the lab identified 794 positive tests based on a threshold of 40 cycles. With a cutoff of 35, about half of those tests would no longer qualify as positive. About 70 percent would no longer be judged positive if the cycles were limited to 30. In Massachusetts, from 85 to 90 percent of people who tested positive in July with a cycle threshold of 40 would have been deemed negative if the threshold were 30 cycles, Dr. Mina said. “I would say that none of those people should be contact-traced, not one,” she said.
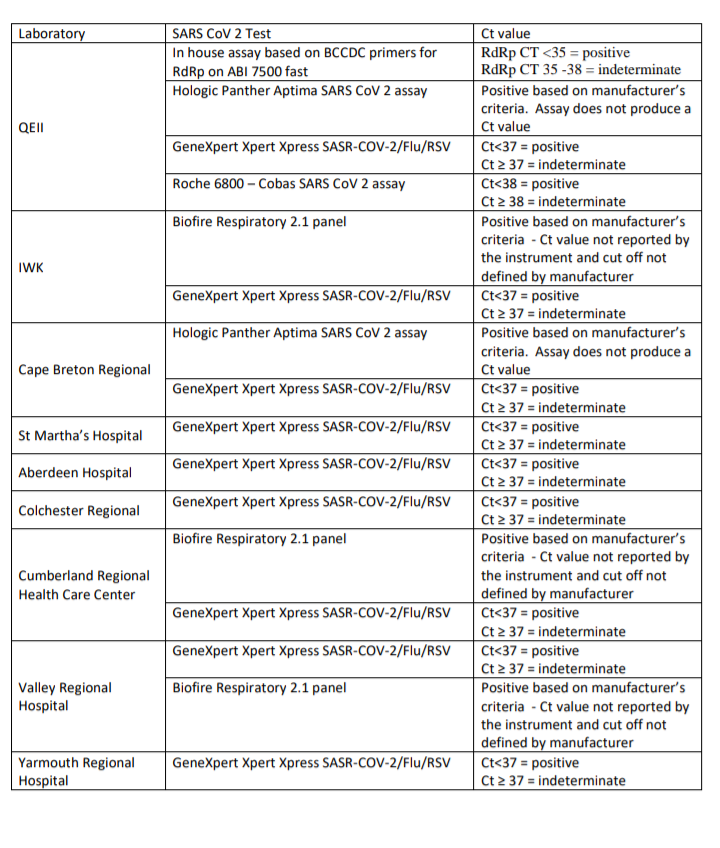
Nova Scotia PCR Test Data
In March, 2021, a freedom of information request (NSHA-2021-33) was filed, requesting information regarding PCR tests and cycle thresholds in Nova Scotia between March 2020 and March 2021. The PCR cycle threshold used in NS ranges from 34-37. There is no explanation as to why it varies, other than each lab, of which there are 16 spread across 9 sites in NS, has their own test and associated cycle threshold (see image below). It appears the (presumably) main lab at the QEII is the only lab with an in house test (not one that is purchased from a third party) and that is the only test with a 34 cycle threshold (35-38 is considered indeterminate). All others are 36, 37 or aren't listed, which we assume means the test is self contained and simply gives a positive or negative result and the cycle threshold is set by the manufacturer of the test and is not noted.
The average cycle threshold required to diagnose a positive case since March, 2020 is 26.9. The percentage of all positive cases that required a cycle threshold greater than 30 is 35%. During the time frame covered by this data, there were approximately 1700 positive test results. If 35% of those were diagnosed at 31 or more PCR cycles, that is nearly 600 cases that should have never been classed as a case. That's a lot of people that had to isolate for 14 days unnecessarily (and all the impacts that go along with that) because of the way we use PCR tests and the refusal of our medical professionals and politicians to do anything other than a "better safe than sorry", one size fits all approach.